Understanding the Difference between Medi-Cal and Covered California
Today we are going to delve into the difference between Medi-Cal and Covered California. Understanding the difference between these two programs is essential to make an informed decision about your health coverage.
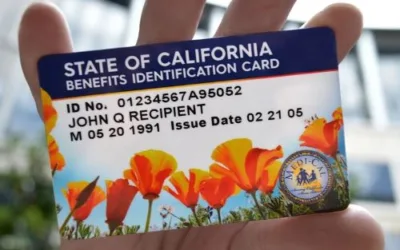
Medi-Cal
Medi-Cal is a public health insurance program providing free or low-cost health care coverage to low-income adults, families with children, seniors, persons with disabilities, pregnant women, children in foster care, and low-income people with specific diseases such as tuberculosis, breast cancer, or HIV/AIDS.
- Eligibility: Primarily based on your income, family size, disability status, and other specific factors. You can apply at any time of the year.
- Cost: Most Medi-Cal services are provided at no cost to the recipient, although there may be a small co-pay for some services, depending on your income and the service provided.
- Coverage: Both Medi-Cal and Covered California plans are required to provide Essential Health Benefits. This ensures that no matter which program you qualify for, you have access to a broad spectrum of basic healthcare services.
Covered California
On the other hand, Covered California is a marketplace for private insurance under the Patient Protection and Affordable Care Act (ACA). It provides a platform for individuals and small businesses to compare and purchase health insurance plans, often with the benefit of federal tax credits and subsidies to make insurance more affordable.
- Eligibility: Open to all residents who don’t have access to affordable health insurance through their employer or another government program. The key enrollment period is typically at the end of the year during Open Enrollment, although Special Enrollment periods can occur due to life-changing events.
- Cost: Costs vary widely based on the plan selected, your income, and family size. However, federal tax credits and subsidies are available to lower-income individuals and families, which can significantly reduce these costs.
- Coverage: The coverage varies based on the plan chosen, but all plans cover essential health benefits as defined by the ACA, including preventive and wellness services, mental health services, emergency services, prescription drugs, and more.
When you apply through Covered California, the application process includes a review for Medi-Cal eligibility. This is because both programs are structured to provide health coverage based on income and family size, albeit in different ways.
Let’s consider a scenario for clarity:
Suppose you’re a single adult with an income that fluctuates around the Medi-Cal income limit. If your income drops, you might become eligible for Medi-Cal, which provides low-cost or free health coverage. If your income increases, putting you above the limit for Medi-Cal, you may no longer be eligible for Medi-Cal. However, you could still be within the income range to qualify for premium subsidies on a health plan purchased through Covered California.
The ultimate goal of both programs is to ensure that all Californians have access to affordable, quality health care. Regardless of your age, health, or financial status, there is a plan out there that can meet your needs. The important thing is to research, understand your options, and select the right plan for you and your family.
Essential Health Benefits
While it’s crucial to understand the differences between Medi-Cal and Covered California, it’s equally important to know what they have in common. One significant similarity lies in the coverage of Essential Health Benefits as mandated by the Affordable Care Act (ACA). Both Medi-Cal and Covered California plans all include Essential Health Benefits.
What Are Essential Health Benefits?
Essential Health Benefits are a set of 10 categories of services that every health insurance plan must cover under the ACA. These categories aim to ensure that everyone has access to basic healthcare services, from preventive care to emergency treatments. The ten categories are:
- Ambulatory Patient Services: Also known as outpatient care.
- Emergency Services: Treatment in an emergency room.
- Hospitalization: Treatment in a hospital for inpatient care.
- Maternity and Newborn Care: Care before and after your baby is born.
- Mental Health and Substance Use Disorder Services: Includes behavioral health treatment, counseling, and psychotherapy.
- Prescription Drugs: At least one prescription drug must be covered for each category of federal drug classes.
- Rehabilitative and Habilitative Services and Devices: Help recovering skills lost because of injury, disability, or a chronic condition (rehabilitative), or help acquire new skills (habilitative).
- Laboratory Services: Testing to help diagnose injuries, illnesses, or conditions.
- Preventive and Wellness Services and Chronic Disease Management: Immunizations, screening tests, and treatments aimed at managing a chronic disease.
- Pediatric Services: Includes oral and vision care for children.
Coverage Across Programs
Both Medi-Cal and Covered California plans are required to provide these Essential Health Benefits. This ensures that no matter which program you qualify for, you have access to a broad spectrum of basic healthcare services.
Extent and Cost Variations
While both programs cover these essential services, the extent and cost to the enrollee may vary. Medi-Cal, being an assistance program, often covers these services at a lower cost or even free for eligible enrollees. On the other hand, Covered California plans may require copayments, deductibles, or coinsurance for the same services.
Limitations and Special Conditions
Each program may have limitations or special conditions for these essential benefits. For instance, some Medi-Cal plans may require prior authorization for certain services. Covered California plans may have limitations on which providers you can see for these services to be covered.

Eligibility Criteria: Navigating the Numbers for Medi-Cal and Covered California
When it comes to healthcare, understanding eligibility criteria is a crucial first step. Medi-Cal and Covered California both offer valuable options, but they target different income levels, age groups, and special circumstances like pregnancy. Here’s what you need to know:
Income Levels and Age Factors
Medi-Cal
- Adults: If you’re over the age of 19, you may qualify for Medi-Cal if your income doesn’t exceed 138% of the Federal Poverty Level (FPL).
- Children: The eligibility criteria for kids are a bit more lenient. Children between the ages of 0-18 can qualify for Medi-Cal if the household income is up to 266% of the FPL.
- Pregnant Women: Medi-Cal offers specialized programs for expectant mothers. If you’re pregnant and your income is between 138% and 213% of the FPL, you could qualify for Medi-Cal for Pregnant Women. For those with incomes above 213% and up to 322% FPL, the Medi-Cal Access Program for Pregnant Women becomes an option.
Covered California
- Eligibility for Covered California is generally for those who have incomes between 138% and 400% of the FPL. This makes it a viable option for those who might earn too much to qualify for Medi-Cal but still need financial assistance for healthcare coverage.
- Furthermore, if your income surpasses 400% of the FPL, you’re not left out; a new subsidy is available that limits your healthcare premiums to 8.5% of your income for eligible Silver Plans. This offers substantial financial relief for households with higher incomes.
Find Your Eligibility Based on Household Income: Use the Table Below
Navigating healthcare options can sometimes feel like a maze. To simplify the process and help you identify which program you may qualify for, we’ve prepared a table below. This table breaks down eligibility criteria based on household income levels for both Medi-Cal and Covered California.
Take a moment to locate your household income range in the table to see which healthcare program you or your family may be eligible for. This easy-to-use resource aims to streamline your decision-making process, saving you both time and effort as you seek the most suitable healthcare coverage.
Federal Poverty Level Chart (2024)
The Affordable Care Act (ACA) Impact
The ACA significantly expanded the reach of healthcare programs. It broadened Medi-Cal’s eligibility criteria and created Covered California to provide a marketplace for affordable insurance. The income brackets mentioned above (like 138% FPL for adults in Medi-Cal or 400% FPL for Covered California) are a direct result of the ACA’s guidelines.
Wrapping It Up
Understanding these eligibility criteria will help you identify which healthcare program best suits your needs or those of your family. Whether it’s Medi-Cal’s broader scope for lower-income households or the wider array of options under Covered California for middle-income earners, both programs have their distinct advantages and limitations.
By examining these factors closely, you can make a more informed choice, ensuring that you or your loved ones have the healthcare coverage that best fits your situation.
This article was written by Mark Svetlik, with the assistance of automation technology. The content has undergone thorough editing and fact-checking to ensure complete accuracy.