Understanding Covered California Subsidy Payback: What to Do When Your Income increases or decreases
Life can be unpredictable. Incomes increase and decrease, careers change, and financial surprises can appear out of nowhere. One area where these surprises can have significant implications is in the case of health insurance tax credits.
For our clients at our Covered California Enrollment Center, it’s extremely important to understand the implications of these changes, especially when it comes to federal tax credits.
Let’s explore the story of Steve as a case study.
Steve’s Journey with the Silver Plan
Steve started his year by enrolling in a subsidized health insurance plan through Covered California. Midway through the year, Steve’s financial fortunes rose, but he missed a crucial step: notifying Covered California of this change.
Why Reporting Income Changes Matters
Subsidies are financial aids extended by the government, helping eligible individuals offset their health insurance premiums. These subsidies are calculated based on one’s Modified Adjusted Gross Income (MAGI). they are directly linked to one’s annual income. Therefore, ensuring that assistance is provided in accordance with an individual’s financial capacity. Falling below the federal poverty level might even qualify you for Medi-Cal, California’s version of Medicaid.
But what happens if, like Steve, your income shifts during the year?
- Income Increases: If your actual earnings surpass your estimates, you may need to return a portion or all the subsidy you were granted.
- Income Decreases: On the flip side, a drop in income can make you eligible for further financial assistance.
Notably, if someone with a Covered California Subsidized Plan experiences a significant income surge, they might need to repay some or all of the received subsidy. However, there’s a silver lining: a repayment cap. For those with earnings below 400% of the federal poverty level, the repayment amounts range from $325 to $1,400 for single tax filers and $650 to $2,800 for families. The exact repayment depends on your income. Please refer to the repayment schedule below for detailed information.
The Importance of Prompt Reporting
Failing to report income changes in a timely manner may have a negative impact on your taxes if you are receiving a tax credit. When you file your income tax return you may end up with an unfortunate tax liability. Additionally, there is a possibility you may have to repay the full amount of the subsidy you received. By staying informed and proactive you can avoid any unnecessary surprise at tax time and maximize your healthcare benefits.
It’s crucial for all Covered California enrollees to be aware of the implications of income changes on their health insurance coverage. If you experience a change in income, it’s imperative to report it promptly to Covered California.
What if I Overestimate My Income for Covered California
If you find that you’ve overestimated your income when enrolling in a Covered California plan, it can have significant implications for your healthcare subsidies. Overestimation typically means you received less in subsidies than you were actually eligible for. Consequently, this may lead to a pleasant surprise at tax time, where you could be entitled to a credit or a larger refund to compensate for the underutilized subsidies. An income decrease might have two notable benefits:
- Reduction in Monthly Premiums: By promptly reporting a decrease in income, you could be eligible for a higher subsidy, effectively lowering your monthly health insurance costs.
- Enhanced Plan Benefits: With a decreased income, you may also qualify for (Cost-Sharing Reduction Plans). CSR plans are designed to reduce your out-of-pocket healthcare expenses for individuals and families that qualify based on household income.
Tax Filing Status and Covered California Subsidy Repayment
It is important to understand how your tax filing status can affect your federal tax credit repayment. Alongside the risk of having to return your advanced tax credit due to an income increase that wasn’t reported, this obligation also applies if you file as ‘Married Filing Separately.’
In this scenario, you’ll need to return the entire advanced tax credit you received, a requirement that complies with both state and federal rules. The implications can be financially substantial, so it’s key to factor in this aspect when making healthcare and tax-related decisions. As always, seeking personalized advice from a tax professional can help you navigate these complexities effectively.

Understanding Subsidy Paybacks Through Real-Life Scenarios
Navigating the nuances of Covered California’s subsidy payback system can be a bit challenging, especially when tax season approaches. Let’s dive into some real-life scenarios of our clients to help clarify how these rules apply:
- Mary’s Fortunate Miscalculation:
- Initial Estimate: Mary started her year estimating her annual household income at $42,000.
- Actual Earnings: By year’s end, she only earned $25,000.
- Monthly Subsidy Reality: Mary received a monthly subsidy of $533.00 based on her initial estimate.
- What Could Have Been: If she had estimated accurately, Mary would have been entitled to a monthly subsidy of $742. Additionally, She would have qualified for an Enhanced Plan with lower out-of-pocket cost.
- Tax Season Outcome: Due to her overestimation, Mary received a tax refund of $2,508 (the difference of $209 for each month she was under the health plan).
- Jeff’s Fortunate Break:
- Initial Estimate: Jeff anticipated his yearly income to be around $29,000.
- Actual Earnings: By the close of the year, he amassed earnings of $40,500.
- Subsidy Implications: Jeff’s miscalculation would have resulted in a repayment of $1,656. However, thanks to the subsidy payback cap and his income landing within the 200%-300% FPL range, he was only obligated to return $825.
- Miguel and Maria’s Pricey Oversight:
- Initial Estimate: This couple began their year with an estimated household income of $65,000.
- Actual Earnings: When tax season arrived, their reported income jumped to $98,000.
- The Costly Oversight: Since Miguel and Maria did not report their income increase to us, they were ineligible for the subsidy at tax time. Additionally, with their income exceeding the 400% FPL threshold, they were obligated to return the full subsidy amount, totaling $5,492.
It’s essential to note the importance of promptly updating income changes with Covered California. While some like Mary might walk away with an unexpected refund, others, like Miguel and Maria, might face substantial repayments. Always stay informed to avoid financial surprises.
Additional Resources
For a detailed look at the limits on repayment amounts and Federal Poverty Levels based on household size, refer to the “Subsidy-Repayment Limits below” and “Federal Poverty Level-2024” tables, respectively.
Did your income change this year? Don’t wait. Reach out to us now to update your details and ensure you’re receiving the correct subsidies.
For more in-depth information and resources, we welcome you to visit our website or contact us at (888) 280-0763.
Subsidy Repayment Cap (2023)
Federal Poverty Level Chart (2024)
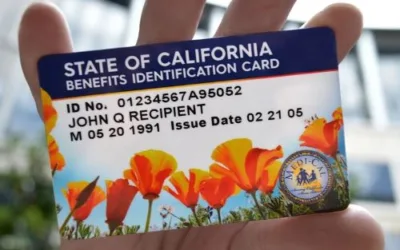
Penalty for Not Reporting Income to Medi-Cal
One of the most critical aspects of maintaining your Medi-Cal benefits is ensuring that your income information is up-to-date and accurately reported. Medi-Cal, California’s Medicaid program, offers health coverage to eligible individuals and families with low incomes and resources. It is vital to understand the repercussions of not reporting income changes, as it can lead to significant penalties.
Why Accurate Reporting Matters
Medi-Cal eligibility is largely based on your income level. When there are changes in your income, whether it’s an increase or decrease, it directly impacts your eligibility and the benefits you are entitled to receive. Not reporting these changes can be considered a form of fraud, as it may result in receiving benefits that you are no longer eligible for.
Consequences of Not Reporting
- Benefit Adjustments or Cancellations: The most immediate consequence is the adjustment or termination of your benefits. If Medi-Cal discovers income discrepancies, they may retroactively cancel your coverage or modify it to reflect your actual income level.
- Repayment of Benefits: You may be required to repay the benefits you received while your income was inaccurately reported. This repayment can be a substantial financial burden, especially if the unreported income period is extensive.
- Legal Repercussions: In severe cases, not reporting income to Medi-Cal can lead to legal actions. This includes charges of fraud, which can result in fines and even criminal prosecution, depending on the severity of the offense.
- Impact on Future Eligibility: Your future eligibility for Medi-Cal and other government assistance programs can be affected. Having a record of misreporting income can lead to increased scrutiny in future applications or renewals for any form of government aid.
How to Report Income Changes
To avoid these penalties, it’s crucial to report any changes in your income as soon as possible. You can report income changes to Medi-Cal through your local county social services office, either in person, by phone, or in some counties, online. It’s recommended to keep records of your communications regarding income updates to ensure there’s a record of your compliance.
Conclusion
Staying compliant with Medi-Cal’s reporting requirements is not just about following the rules; it’s about maintaining the integrity of the system that provides essential healthcare services to millions of Californians. By accurately reporting your income, you are ensuring that these valuable resources are allocated fairly and to those who truly need them.