Covered California and Medi-Cal for Pregnant Women: Options, and Benefits
Pregnancy is a beautiful and transformative time in a woman’s life, bringing with it a mix of joy, anticipation, and inescapably, some anxiety. One major cause of stress can be understanding and managing healthcare coverage. But worry not, Covered California is here to ensure you and your little one are taken care of, both before and after birth. Here’s how you can navigate the options, benefits, and procedures for expectant mothers in California.
The Importance of Health Coverage During Pregnancy
Access to quality healthcare is crucial during pregnancy. Regular prenatal checkups help doctors monitor both the mother and the baby’s health, catching potential problems early and ensuring a healthy pregnancy. Health coverage also protects you financially from unforeseen complications that can lead to high medical costs.
Covered California, the state’s health insurance marketplace, helps Californians find affordable, high-quality health insurance. If you’re an expectant mother, you may be wondering about the specifics of how this works for you.
Qualifying for Coverage
Having a baby is a significant moment in life, and it’s considered a “qualifying life event” under the Affordable Care Act (ACA). This means that you can apply for or change your health plan outside of the usual Open Enrollment Period upon the birth of your baby.
It’s important to note that while becoming pregnant is a monumental life event, it does not, in itself, qualify you to apply for a health plan during a Special Enrollment Period. However, California offers several programs that provide support to expectant mothers, ensuring that you have access to necessary healthcare services during this crucial time.
Options for Expectant Mothers
Enrollment in a Covered California health plan is typically available only during Open Enrollment periods or through Special Enrollment triggered by specific life events. It’s important to note that becoming pregnant does not qualify you for Special Enrollment. Despite this limitation, all health plans offered through Covered California provide essential benefits tailored to the needs of expectant mothers. These benefits include comprehensive coverage for prenatal care, labor, delivery, and care for your newborn. In addition, preventive services such as breast pumps for nursing mothers are covered without any extra charges. You have the option to compare various health plans to find the one that best fits your needs, taking into account coverage options, costs, and the availability of doctors and hospitals within the plan’s network.
During the enrollment process, you’ll be asked whether you are pregnant. Your answer has important implications for the types of plans you may qualify for.
Why Does Pregnancy Matter?
By indicating that you are pregnant on the application, Covered California’s system will automatically consider your eligibility for Medi-Cal programs specifically designed for pregnant women. This is crucial because Medi-Cal may provide more comprehensive benefits for prenatal and postnatal care.
Dual Eligibility for Couples
Based on your income and family situation, it’s possible for the spouse to qualify for a subsidized Covered California plan while the pregnant wife may be eligible for a Medi-Cal plan. This dual eligibility allows families to maximize their benefits and ensure both parents-to-be are covered adequately.
What Happens After Birth?
It’s important to note that eligibility for Medi-Cal may change after the birth of your child. The birth mother may lose her Medi-Cal coverage and become eligible for a Covered California plan instead. It’s vital to update your information with Covered California after the birth to reassess your options.
Navigating health insurance options can be complex, especially with a new family member on the way. Make sure to consult with enrollment experts to explore the best health coverage options for you and your growing family.
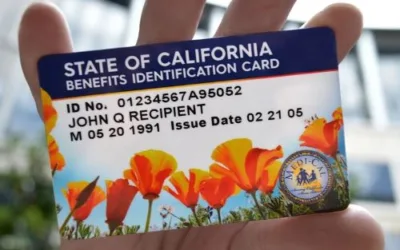
Medi-Cal
Medi-Cal is a program that offers low-cost or free health coverage for Californians with limited income. Pregnant women are covered for prenatal care, labor, and delivery, and care after birth. Even if you don’t qualify for Medi-Cal based on your income, you may qualify based on your pregnancy. The program includes income adjustments that essentially increase the income limit for pregnant women, making it easier for more people to qualify.
Medi-Cal Access Program (MCAP)
Formerly known as the Access for Infants and Mothers program, the MCAP offers low-cost coverage for pregnant women who don’t qualify for no-cost Medi-Cal without a share of cost. If your income is too high for Medi-Cal, MCAP could be a good option. It covers all medically necessary pregnancy-related services from conception through 60 days postpartum.
Applying for Coverage
To apply for coverage, you can visit a Covered California Enrollment Center or fill out an application on the Covered California website. This application will check if you qualify for Covered California health plans with premium assistance, or for low-cost or no-cost coverage through Medi-Cal or the MCAP.
After you’ve submitted the application, you’ll receive an eligibility notice letting you know which programs you qualify for. If you qualify for a Covered California health plan, you’ll also see a list of plan options and their costs. You can then choose a plan that fits your needs and budget.

Program Eligibility by Income
Covered California for Pregnancy
- Income Eligibility: Tax credits to help offset the cost of plans are available for individuals with incomes ranging from above 138% to up to 400% of the Federal Poverty Level (FPL). In certain cases, these tax credits may be extended beyond the 400% FPL threshold.
- Coverage Benefits: Offers essential health benefits such as prenatal care, labor, delivery, and newborn care. Preventive services are also covered without additional costs.
- Limitations: Depending on your chosen plan, you may be required to pay co-pays or meet a deductible.
- Extra Perks: You may be eligible for premium assistance based on your income.
- Special Enrollment Period: You can apply for or change your health plan upon the birth of your child.
Standard Medi-Cal
- Income Eligibility: For those with incomes up to 138% of FPL.
- Coverage Benefits: Comprehensive coverage including prenatal care, labor, delivery, and postnatal care.
- Limitations: You may have a limited choice of doctors and hospitals.
- Extra Perks: Offers low-cost or free coverage.
- Special Enrollment Period: Your eligibility is automatically reviewed for continued coverage.
Medi-Cal for Pregnant Women
- Income Eligibility: For pregnant women with incomes above 138% and up to 213% of FPL.
- Coverage Benefits: Offers the same comprehensive coverage as Standard Medi-Cal, but tailored for pregnancy needs.
- Limitations: Limited network of doctors and hospitals, similar to Standard Medi-Cal.
- Extra Perks: Also offers low-cost or free coverage.
- Special Enrollment Period: Automatically reviewed for continued eligibility post-pregnancy.
Medi-Cal Access Program (MCAP)
- Income Eligibility: For those with incomes above 213% and up to 322% of FPL.
- Coverage Benefits: Focuses on pregnancy-related services from conception through 60 days postpartum.
- Limitations: Exclusively covers pregnancy-related services and may have a higher income cap compared to both Medi-Cal options but lower than Covered California.
- Extra Perks: Provides low-cost coverage for those who do not qualify for no-cost Medi-Cal.
- Special Enrollment Period: Coverage extends through 60 days postpartum.
Federal Poverty Level Chart (2024)
Postpartum Coverage: Transitioning from Medi-Cal to Covered California
While pregnancy can make you eligible for Medi-Cal for Pregnant Women if your income is above 138% of the Federal Poverty Level (FPL), or Medi-Cal Access Program if your income exceeds 213% FPL it’s essential to understand that this eligibility may change after your child is born. Once you are no longer pregnant, you may find that you no longer qualify for Medi-Cal based on your income. In this case, you will need to transition to a Covered California health plan to maintain your healthcare coverage.
What Happens to Your Newborn’s Coverage?
Depending on your household income, your newborn may qualify for different types of coverage. Your child may be eligible for Medi-Cal, even if you are not, due to different income guidelines for infants. Alternatively, your newborn could also be covered under a family plan through Covered California, depending on your eligibility and income.
To ensure a smooth transition and continuous coverage for both you and your newborn, it’s advisable to review your options and initiate any necessary changes as soon as possible after your child’s birth. Remember, the birth of your child qualifies as a “Special Enrollment Period,” allowing you to make changes to your health plan outside of the regular Open Enrollment period.
Understanding these shifts in coverage options postpartum can help you prepare for any adjustments you’ll need to make, ensuring that both you and your new addition are adequately covered.

FAQs for Pregnancy and Health Coverage
Navigating health coverage options during pregnancy can be overwhelming. We’ve gathered some frequently asked questions that expectant mothers often have about applying for Covered California, Medi-Cal, and other programs.
1. Can I apply for Covered California if I’m pregnant?
Yes, you can apply for Covered California. However, it’s important to note that pregnancy itself is not considered a qualifying life event for a Special Enrollment Period. You can enroll during the Open Enrollment period or if you experience another qualifying life event, such as a change in income or marital status.
2. What happens to my health coverage after my baby is born?
The birth of your baby is considered a qualifying life event, which means you can apply for or change your health coverage. Depending on your income, you may qualify for a Covered California plan or Medi-Cal.
3. Are prenatal and postnatal care covered under Covered California?
Yes, all health plans offered through Covered California include essential health benefits like prenatal care, labor, delivery, and newborn care. Preventive services, such as breast pumps for nursing mothers, are also covered without additional costs.
4. Can I qualify for Medi-Cal while I’m pregnant?
Yes, Medi-Cal has specific provisions for pregnant women. Depending on your income, you may qualify for the Standard Medi-Cal program or the Medi-Cal for Pregnant Women program.
5. What is the Medi-Cal Access Program (MCAP)?
MCAP is a program designed for pregnant women who don’t qualify for no-cost Medi-Cal but still require affordable health coverage. The program focuses on pregnancy-related services and extends coverage through 60 days postpartum.
6. How do I know which program I qualify for?
Your eligibility primarily depends on your income level in relation to the Federal Poverty Level (FPL). We’ve included an FPL chart in this post to help you identify which program may be most suitable for you.
7. How do I apply for health coverage?
You can apply for coverage by calling or visiting a Covered California Enrollment Center or through the Covered California website, which will also check your eligibility for Medi-Cal programs. Once your application is reviewed, you’ll receive an eligibility notice with information on the programs and plans you qualify for.
This article was written by Mark Svetlik, with the assistance of automation technology. The content has undergone thorough editing and fact-checking to ensure complete accuracy.